19 Evidence-based practice, quality assurance and quality improvement in healthcare
Evidence-based practice (EBP) and quality assurance (QA) are two fundamental pillars of modern healthcare; included in QA approaches are quality improvement (QI) tools which we discuss later in this section. Both EBP and QA approaches play crucial roles in ensuring that medical interventions are safe, effective, and patient-centered. In the following, we explore the significance of EBP and QA concepts (including the different types of Quality Improvement activities) and how they contribute to the delivery of high quality healthcare.
Firstly, we will explore how EBP and QA support the integration of evidence into the delivery of healthcare and ensure that high quality patient centered care is the focus of the health care team.
Evidence-based practice (EBP)
Evidence-Based Practice (EBP) is the systematic based approach to identify and integrate the best available research, clinical expertise, and patient preferences that guide high quality clinical decision-making. It emphasises the critical evaluation of and application of research findings, clinical trials, and patient outcomes to inform potential medical interventions and treatment options. EBP seeks to align care delivery with current and validated evidence to improve patient outcomes, enhance patient safety, and ensure the delivery of effective, efficient, and patient-centred care. Incorporating both research and healthcare professionals’ expertise, EBP promotes a holistic and informed approach to patient management while continually adapting to emerging research (Sackett et al, 1996). Clinical practice guidelines are often compiled by expert teams and advisory groups to ensure that the latest clinical guidance based on the best available evidence is available to clinicians and patients to inform care delivery. Benefits include improved consistency and reduced variation in planned care for patients with similar conditions and procedures, as well as the opportunity to include patient preferences for their health care. Clinical guidelines are updated to include latest research and ensure healthcare is based on contemporary evidence. The Queensland State Government produces a number of clinical guidelines focused on maternity and neonatal, adult diabetes and others along with resources to support the development and review, governance and administrative support in development of clinical guidelines. The aim of clinical guidelines team is translating evidence into best clinical practice. Visit the Queensland Clinical Guidelines.
Clinical guidelines activity
Quality assurance (QA)
In addition to EBP, the role of Quality Assurance (QA) in healthcare is to provide a systematic and continuous process of monitoring, evaluating, and improving healthcare practices to ensure they meet established standards of safety, effectiveness, and quality of health care delivery. QA encompasses various strategies and Quality Improvement (QI) activities aimed at preventing errors, identifying areas for enhancement, and promoting optimal patient care. Through ongoing assessment of actual care compared to best care, data analysis, and performance measurement, QA seeks to minimise variations in care, reduce medical errors, and enhance patient outcomes (National Academies of Sciences, Engineering, and Medicine, 2015).
The methods used by the QA process will be specific to each activity, and so will the number of QI tools specific to each approach. Quality Improvement (QI) activities are the tools used to evaluate healthcare is delivered in a systematic and collaborative manner that promotes the quality, safety, and efficiency of healthcare services (Berwick 2008). QI activities involve continuous assessment, analysis of data, identification of areas for enhancement, and implementation of interventions to achieve better patient outcomes and satisfaction. It aims to optimise processes, minimise errors, and align practices with evidence-based guidelines, leading to improved healthcare delivery and patient-centred care. This process can help to identify areas for improvement as well as where best practice is implemented the features of high-quality health care providers (Berwick, Nolan, & Whittington, 2008).
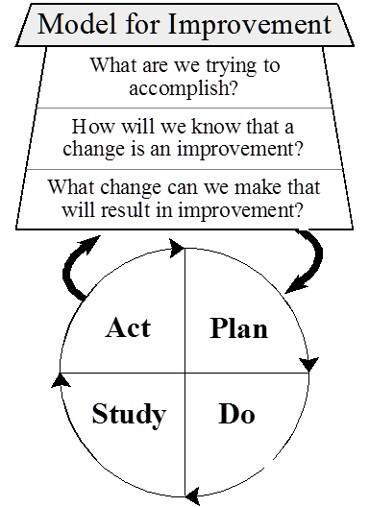
The Plan-Do-Study-Act approach provides an iterative approach for continuous improvement. This approach is frequently applied in healthcare when reviewing processes related to person and clinical care, in order to identify approaches to resolve issues, evaluate the impact of change, and ultimately improve patient outcomes and enhance the quality of care.
Safety and quality reporting
In Australia, the National Safety and Quality Health Service (NSQHS) Standards provide a nationally consistent statement of the level of care consumers can expect from health service organisations. These Standards were developed by the Commission in collaboration with the Australian Government, states and territories, private sector providers, clinical experts, patients and carers. The primary aims of the NSQHS Standards are to protect the public from harm and to improve the quality of health service provision. Frameworks and reporting resources are provided to support QI activities at a local level and may contribute to health care service reaccreditation. Undertaking QA and QI activities in healthcare provides evidence of the importance of quality of health care and a commitment to ensure delivery of quality health care regardless of the health care setting.
Australian Institute of Health and Welfare
The Australian Institute of Health and welfare (AIHW) reports on the quality and safety of Health care provided in both public and privately funded organisations in Australia. To provide the highest quality health care requires that we reflect on our health care practices and their impact. Identifying variation in care delivery, whether geographical or clinician based helps to identify the best outcomes for patients and reduce harm. The AIHW Health Atlas series commenced in 2015 and provides detailed reporting on focused health care topics, variation in health care delivery and possible reasons for variation in care with actions to reduce unwarranted variation.
Publicly available reports are provided that enable reporting and tracking of data to ensure the timely, equitable and efficient delivery of health care resources. Comparisons can be made between jurisdictions to ensure that best practice is available to all and that agreed on benchmarks are adopted to evaluate current practice.
Internationally, The World Health Organization (WHO) Quality of care leads the global community in reporting on health care delivery data and health care outcomes between countries with the Health Outcomes Atlas. It is noted that health care delivery varies between developed and developing countries and countries with universal versus user pays health care.
Benefits of EBP and QA approach
While closely related, Quality Assurance (QA) provides additional benefits through the exploration of care delivery.
Synergy between EBP and QA
The synergy between evidence-based practice and quality assurance is evident in their shared focus on delivering the best possible care to patients:
- Enhancing patient-centred care: Both EBP and QA prioritise patient preferences and needs. EBP ensures that interventions align with patient values, while QA practices work to create a safe and supportive environment for patients.
- Continuous learning and improvement: EBP and QA both emphasise continuous learning and improvement. EBP encourages healthcare professionals to stay updated with the latest research, while QA promotes ongoing assessment and refinement of healthcare processes.
- Reducing errors and improving outcomes: EBP helps identify effective interventions, reducing the likelihood of errors caused by outdated or unproven practices. QA practices further enhance patient safety by minimising errors and improving overall outcomes.
- Accountability and transparency: Both EBP and QA practices promote accountability and transparency within healthcare systems. EBP relies on transparent reporting of evidence, while QA ensures that healthcare organisations are accountable for the quality of care they provide.
- Data-driven decision-making: Both concepts rely on data analysis to inform decision-making. EBP relies on research data to guide clinical choices, while QA uses data to assess and improve the quality-of-care delivery.
In essence, evidence-based practice and quality assurance are complementary approaches that work together to ensure that healthcare delivery is based on the best available evidence, adheres to standardised protocols, and prioritises patient safety and well-being. Their significance lies in their collective ability to drive healthcare practices that are effective, efficient, safe, and patient-centred. When considering the quality of health care, a number of factors about how effective, safety and if care is patient focused needs consideration. The World Health Organization quality of care considers how effective, safe and patient-centred care.
Limitations of EBP and QA approach
While evidence-based practice (EBP) is a widely accepted and effective approach to healthcare decision-making, it is not without its limitations. One fundamental flaw of EBP is often referred to as the “EBP Implementation Gap” or the “Research-to-Practice Gap.” This gap highlights the challenge of effectively translating research evidence into clinical practice and the real-world care of patients.
Limitations can include the delay in incorporating new evidence into clinical practice. This can be the result of new studies and evidence. However, the systematic review process of reviewing, validating, and disseminating new evidence can be time-consuming. As a result, there may be a lag between the publication of new research and its widespread incorporation into clinical guidelines. The evidence that is available may not provide meta-analysis or high-level summaries and consideration of the quality of the study in terms of quality, methodology and evidence can also influence health care. This diversity of evidence sources, quality and applicability can make it challenging to determine the best course of action.
Clinical practice is complex and needs to consider the patient and their preferences. Clinical decision making is further influenced by patient preferences, comorbidities, socio-economic status and resources that are unique to each case.
Human and organisational factors also influence clinical decisions. They are influenced not only by evidence but also by cognitive biases, institutional policies, time constraints, and resource availability. Healthcare professionals may be hesitant to change established practices, even in the presence of compelling evidence.
Lack of applicability: Some research findings might not be directly applicable to all patient populations or clinical scenarios. Studies often have inclusion and exclusion criteria that limit their generalisability to real-world settings, causing uncertainty about whether the findings can be applied to diverse patient groups.
Consequences of the flaw
The gap between research evidence and clinical practice can lead to several consequences:
- Delayed adoption of effective practices: Effective interventions may not be widely adopted in a timely manner, resulting in suboptimal patient care and missed opportunities for better outcomes.
- Overtreatment and undertreatment: In some cases, outdated or ineffective practices might persist, while beneficial interventions might be underutilised due to the slow integration of new evidence.
- Variability in care: The gap contributes to variations in clinical practice, as different healthcare providers and institutions may interpret and apply evidence differently.
Addressing the flaw
To address the implementation gap, healthcare systems need to consider five things.
How to address the flaw
In conclusion, the fundamental flaw of EBP – the research-to-practice gap – underscores the challenges of effectively translating research evidence into clinical care. While EBP offers a systematic approach to decision-making, addressing this flaw requires collaborative efforts among researchers, healthcare professionals, policymakers, and patients to bridge the gap between evidence generation and its application in real-world clinical practice.
Visit Quality of care from the World Health Organization.
Australian Institute of Health and Welfare
In Australia, the Australian Institute of Health and Welfare reports on the quality and safety of Health care provided in both public and privately funded organisations. Reports are provided that enable reporting and tracking of data to ensure the timely, equitable and efficient delivery of health care resources. Comparisons can be made between jurisdictions to ensure that best practice is available to all and that agreed on benchmarks are adopted to evaluate current practice.
Internationally, countries also compare health data and health care outcomes with Atlas. It is noted that health care delivery varies between developed and developing countries and countries with universal versus user pays health care.
Why map care?
To provide the highest quality health care requires that we reflect on our health care practices and their impact. Identifying variation in care delivery, whether geographical or clinical based helps to identify the best outcomes for patients and reduce harm. The AIHW Health Atlas series commenced in 2015 and provides detailed reporting on focused health care topics, variation in health care delivery and possible reasons for variation in care with actions to reduce unwarranted variation.
| Term | Acronym | Definition | Why use | Reference | |
|---|---|---|---|---|---|
| Disability adjusted life years / Morbidity data | DALYs | Time based statistical measure to describe the burden of disease.
Calculates YLLs and YLDs to estimate DALYs impact. One DALY represents the loss of one year of full health |
Provides details of the burdens of disease of individuals and enables calculation of the burden of diseases can be compared between different mortality and morbidity cases. For example, fatal drowning causes premature death (YLLs) and little disability, whereas blindness from preventable cataracts result in low death rates and higher disability (YLDs). | Disability-adjusted life years (DALYs) | |
| Death / Mortality data | YLLs | ||||
| Years of healthy life lost due to disability | (YLDs) |
In conclusion, EBP has been credited with a number of improvement in health care delivery and outcomes. These include improved patient outcomes by integration of the best available evidence, clinical expertise, and patient preferences in decision-making. This approach leads to more informed and effective healthcare interventions, ultimately resulting in improved patient outcomes. QA supports the delivery of quality healthcare by continuous evaluation of current practice and best practice benchmarks to promote quality of healthcare regardless of setting.
Now
After the application of the National Safety and Quality Health Service Standards in 2011, many vital improvements were documented (Australian Commission on Safety and Quality in Health Care, 2017). These included drops in bacteria cases e.g. methicillinresistant S. aureus, lowering of cardiac arrest rates in-hospital and improved adverse drug reaction documentation (Australian Commission on Safety and Quality in Health Care, 2017). Read page 2 of the National Safety and Quality Health Service Standards Accreditation Workbook (PDF, 3.2MB) for other important improvements.
Maternity care
The AIHW (2021) Fourth Atlas of Healthcare Variation explores variation between care providers where planned caesarean births occur 39 weeks gestation without a documented medical or obstetric reason for the birth (Australian Commission on Safety and Quality in Health Care, 2021). Early planned births are associated with poorer outcomes for newborns where there is not a clear indication. This aligned with “every week matters” and the risk to infant developmental outcomes without a documented medical or obstetric indication (REF every week matters). (Australian Commission on Safety and Quality in Health Care, 2021).
Admitted patient safety and quality
The quality of care provided to patients admitted to hospitals can be measured in several ways. One way is to use data from hospitals to measure rates of:
- Staphylococcus aureus (‘golden staph’) bloodstream infections (SABSI)
- Hand hygiene compliance
- Hospital-acquired complications and adverse events
- Potentially preventable hospitalisations (PPHs).
Another way is to survey people about their experiences as hospital patients. Information gathered through hospital data and patient surveys does not cover all aspects of hospital safety and quality. Certain aspects of safety and quality—continuity of care and responsiveness of hospital services—are difficult to measure and are not included here.
This information is from “Admitted patient safety” by Australian Institute of Health and Welfare, published under a Creative Commons Attribution 4.0 licence.
Implementation science
Variation in care, identified in the Atlas Health Variation in Australia (2017) and again in the 2021 version, identifies variation in practice Fourth Atlas 2021 | Australian Commission on Safety and Quality in Health Care
Fourth Australian Atlas of Healthcare Variation
The Whole Nine Months Home – The Whole Nine Months
Example
The Reproductive, Maternal and Newborn Health Clinical Academic Group from Sydney Health Partners.
Objectives of the group include:
- “Harness the research translational and health policy initiatives of all its leading partners and Improve quality of care for women and babies in NSW, by measuring and understanding variations in care.
- Systematically strengthen, develop, and evaluate interventions to reduce unnecessary variations in perinatal care.
- Create the infrastructure and mentorship environment for interdisciplinary capacity and capability building.
- Develop future academic and health service leaders in the field of women’s health and newborn care” (Sydney Health Partners, n.d.).
Their projects include “reduced variations in care leading to pre-term and early-term birth, understanding variations in care leading to preterm and early term birth and developing and implementing best practice interventions” (Sydney Health Partners, n.d.).
Consumers should be at the heart of health care
How can family and carers escalate a response to care if they are concerned?
All Australian hospitals are a part of accreditation with National Safety and Quality Health Service Standards. Ryan’s Rule, available in Queensland Public Hospitals, supports achievement of Standard 9.9 – “Enabling patients, families and carers to initiate an escalation of care response” (Clinical Excellence Queensland, Queensland Health, 2023).
Development of Ryan’s Rule
The formative development of Ryan’s Rule began in 2011, led by Patient Safety and Quality (PSQ) in consultation with hospital and health services (HHSs). In 2013, roll out commenced with Hospital and Health Services provided training for local Ryan Rule coordinators to implement facility based processes. The statewide roll out was completed in 2015. Read the Ryan’s Rule brochure.
Ryan’s Rule exercise
References
Australian Institute of Health and Welfare. (n. d.). Admitted patient safety. https://www.aihw.gov.au/reports-data/myhospitals/intersection/quality/apc/healthcare-associatedstaphylococcusaureusbloodstreaminfections. Creative Commons Attribution 4.0 licence.
Australian Commission on Safety and Quality in Health Care. (2021). Early planned births. https://www.safetyandquality.gov.au/our-work/healthcare-variation/fourth-atlas-2021/early-planned-births
Australian Commission on Safety and Quality in Health Care. (n.d.). National hand hygiene audit data – latest data now available. https://www.safetyandquality.gov.au/our-work/infection-prevention-and-control/national-hand-hygiene-initiative/national-audits-and-hhcapp/national-hand-hygiene-audit-data-latest-data-now-available
Australian Commission on Safety and Quality in Health Care. (2017). National Safety and Quality Health Service Standards accreditation workbook. https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-Accreditation-Workbook.pdf
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The Triple Aim: Care, Health, And Cost. Health Affairs, 27(3), 759-769. https://doi.org/10.1377/hlthaff.27.3.75
Clinical Excellence Queensland, Queensland Health. (2023). Development of Ryan’s Rule. https://clinicalexcellence.qld.gov.au/priority-areas/safety-and-quality/ryans-rule/development-ryans-rule
National Academies of Sciences, Engineering, and Medicine. (2015). Improving diagnosis in health care. National Academies Press.
Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & and W. S. Richardson, W. S. (1996). Evidence based medicine: what it is and what it isn’t. BMJ, 312(7023): 71–72. https://doi.org/0.1136/bmj.312.7023.71
Sydney Health Partners. (n.d.). Reproductive, maternal and newborn health clinical academic group. https://sydneyhealthpartners.org.au/reproductive/

